Feature: Seeking Ways to Crack Cocaine Addiction
The Lancet [Volume 352, Number 9136] 17 October 1998
by Kelly Morris
The use of cocaine, a highly addictive stimulant and euphoriant with few physical withdrawal symptoms, is increasing. Up to 10% of ever-users will become heavy users, particularly if they inject the drug or smoke “crack”, the free base. And many users, notes John Marsden (Institute of Psychiatry, London, UK), do not seek help until they are in crisis, often with financial worries or relationship problems.
Current treatments for addiction can work well, but “there is a high degree of dropout in treatment and a high degree of relapse”, says Frank Vocci (US National Institute on Drug Abuse, Bethesda, MD, USA). Treatment “has traditionally been non-pharmacologically based”, adds Walter Ling (University of California at Los Angeles, CA, USA), although antidepressants such as selective serotonin reuptake inhibitors and desipramine are also used, particularly for the depression, anhedonia, and sleep disturbances that can accompany cocaine withdrawal. With only half of addicts who complete treatment remaining abstinent, the hunt is now on for new treatments.
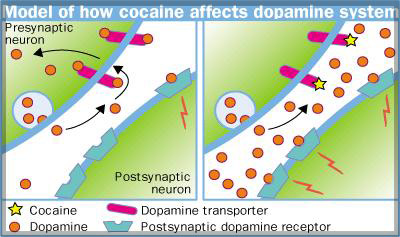
Cocaine blocks the presynaptic dopamine transporter in the mesocorticolimbic dopamine system, increasing synaptic dopamine which is thought to produce the drug’s rewarding effects. Ligands that block the dopamine transporter, especially those with a slow onset and long duration of action, “should increase dopamine levels, possibly block cocaine’s binding to the transporter, and may reduce anhedonia and craving”, explains Vocci. Such drugs include methylphenidate, which is in phase II trials, and two new dopamine-reuptake inhibitors, which are in phase I trials. Phase III trials are planned for selegiline, which reduces dopamine metabolism, and amantadine, which may block dopamine reuptake, adds Vocci.
On the other side of the synapse, dopamine-receptor antagonists could block cocaine’s rewarding effects but might have side-effects. Dopamine-receptor agonists could replace the need for cocaine in a dependent person, but might be addictive themselves, although “a long acting one or a partial agonist may not be”, speculates George Koob (Scripps Research Institute, La Jolla, CA, USA). His team is working on dopamine-receptor partial agonists, such as terguride, which act as antagonists when cocaine is present but which are not reinforcing alone (J Pharmacol Exp Ther 1998; 286: 123138).
For some years, research interest has focused on modulating the dopamine system but with limited success, notes Ling. Several groups, including Koob’s, are approaching addiction from the other end by trying to immunise against cocaine. Antibodies raised to cocaine could stop the drug entering the brain and reduce the user’s high, without the side-effects associated with neurotransmitter manipulation. ImmuLogic (Waltham, MA, USA) has a cocaine-linked hapten in phase I trials. And, a team led by Don Landry (Columbia University, NY, USA) has used catalytic antibodies, which increase cocaine breakdown, to prevent cocaine reinforcement and overdose in rats (Proc Natl Acad Sci USA 1998; 95: 1017681).
The many neurotransmitters that indirectly modify the dopamine system are also potential drug targets. For example, -aminobutyric acid (GABA) reduces synaptic dopamine, so Stephen Dewey (Brookhaven National Laboratory, NY, USA) is investigating vigabatrin, an irreversible inhibitor of the enzyme that breaks down GABA. In August, Dewey reported that vigabatrin stops cocaine increasing synaptic dopamine in baboons and abolishes the preference of animals for an environment associated with cocaine (Synapse 1998; 30: 11929). Vigabatrin is long-acting and does not cause withdrawal effects or tolerance. “Perhaps most importantly, it is not addictive”, says Dewey who is planning to start clinical studies soon.
Deborah Mash (University of Miami, FL, USA) argues that agents that affect several neurotransmitter systems may be the best way to treat addiction. She is testing ibogaine, which is isolated from a plant used by African tribes in religious rituals.
Unable to get funding to complete US phase I trials, Mash has begun residential treatments in St Kitt’s, West Indies. “We were able to show that we can give ibogaine safely . . . patients can be swimming in the Carribean 72 hours later.”
Mash thinks that noribogaine, a metabolite of ibogaine that acts via the serotonin transporter and opioid receptors, is the key to success. So, whether ibogaine works depends on how quickly an addict metabolises the drug. Another factor important for long-term recovery seems to be the “visionary experiences” induced in some patients. “Ibogaine gets you thinking about the nature of your self-destructive behaviour and then the metabolite kicks in to ward off the craving”, says Mash who hopes to develop noribogaine patches as maintenance therapy.
“We’re probably going to find that certain types of drug therapies are optimally suited to particular types of people”, speculates Marsden. But, he says, drug therapies maynot benefit the most chronically affected individuals, who may be unmotivated or hardto reach. An alternative is to use cognitivebehavioural therapy. One approach which is yielding “exciting” results says Marsden, is “contingency contracting”, in which addicts are rewarded for their abstinence with grocery and entertainment vouchers. These seem to act as specific reinforcers, says Ling, who stresses that contingency contracting is not a matter of paying addicts to stay clean, as some critics say. “Addicts will ride across town to give you a clean urine for a few dollars when previously thousands of dollars might have passed through their hands daily from illegal transactions.”
Most researchers agree that combined strategies are needed to beat cocaine addiction. “What we hope for is a therapeutic agent that will provide a window of opportunity for psychosocial and behaviour-modification interventions”, says Landry. For now, Marsden urges the adoption of proven strategies, such as rapid response in crisis and residential programmes. “Science will help us but its not something that we should rest a lot of hope on in the near future”, he warns.




